Journal Articles

Poh, Catherine F; Ng, Samson P; Williams, P Michele; Zhang, Lewei; Laronde, Denise M; Lane, Pierre; MacAulay, Calum; Rosin, Miriam P
Direct fluorescence visualization of clinically occult high-risk oral premalignant disease using a simple hand-held device Journal Article
In: Head & neck, vol. 29, no. 1, pp. 71–76, 2007.
@article{poh2007direct,
title = {Direct fluorescence visualization of clinically occult high-risk oral premalignant disease using a simple hand-held device},
author = { Catherine F Poh and Samson P Ng and P Michele Williams and Lewei Zhang and Denise M Laronde and Pierre Lane and Calum MacAulay and Miriam P Rosin},
url = {https://biophotonics.bccrc.ca/pubs/Poh-2007.pdf, Full Text (PDF)
http://www.ncbi.nlm.nih.gov/pubmed/16983693, PubMed},
doi = {10.1002/hed.20468},
year = {2007},
date = {2007-01-01},
journal = {Head & neck},
volume = {29},
number = {1},
pages = {71--76},
publisher = {Wiley Online Library},
abstract = {A considerable proportion of oral cancer and precancer is not clinically apparent and could contribute significantly to the late diagnosis and high mortality of oral cancer. A simple method to identify such occult change is needed.
METHODS:
Patients in the Oral Dysplasia Clinics at British Columbia are currently being examined with a simple hand-held device that permits the direct visualization of alterations to autofluorescence in the oral cavity. Tissue showing loss of autofluorescence is biopsied.
RESULTS:
We present 3 representative cases in which occult lesions were identified with fluorescence visualization during longitudinal follow-up, resulting in the diagnosis of a primary dysplasia in case 1, a second primary cancer in case 2, and cancer recurrence in case 3.
CONCLUSIONS:
This is the first report of the diagnosis of occult oral disease using a simple noninvasive device. These early examples indicate the potential value of this technology to guide the management of patients with oral lesions, facilitating the detection of high-risk changes not apparent with white-light visualization.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
A considerable proportion of oral cancer and precancer is not clinically apparent and could contribute significantly to the late diagnosis and high mortality of oral cancer. A simple method to identify such occult change is needed.
METHODS:
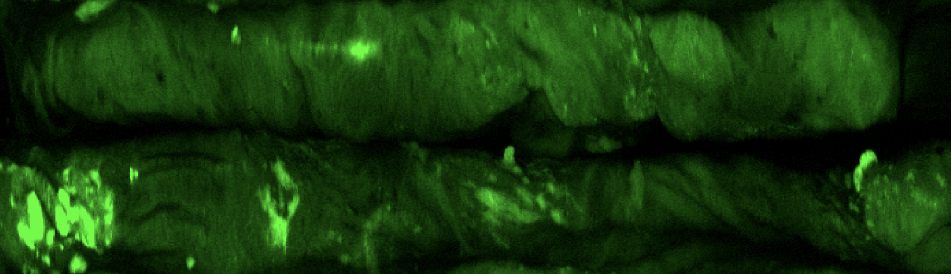
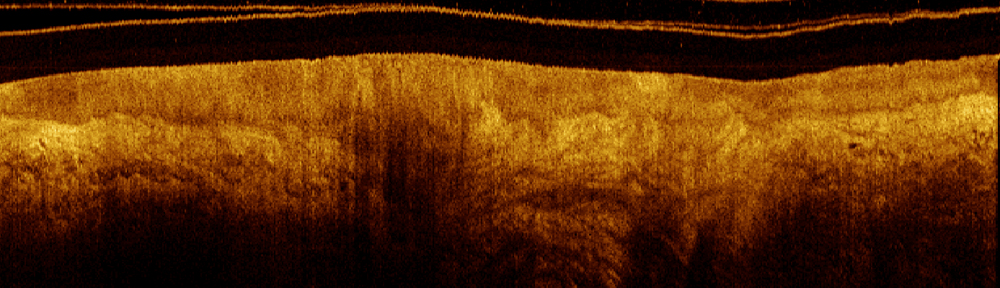
Patients in the Oral Dysplasia Clinics at British Columbia are currently being examined with a simple hand-held device that permits the direct visualization of alterations to autofluorescence in the oral cavity. Tissue showing loss of autofluorescence is biopsied.
RESULTS:
We present 3 representative cases in which occult lesions were identified with fluorescence visualization during longitudinal follow-up, resulting in the diagnosis of a primary dysplasia in case 1, a second primary cancer in case 2, and cancer recurrence in case 3.
CONCLUSIONS:
This is the first report of the diagnosis of occult oral disease using a simple noninvasive device. These early examples indicate the potential value of this technology to guide the management of patients with oral lesions, facilitating the detection of high-risk changes not apparent with white-light visualization.
METHODS:
Patients in the Oral Dysplasia Clinics at British Columbia are currently being examined with a simple hand-held device that permits the direct visualization of alterations to autofluorescence in the oral cavity. Tissue showing loss of autofluorescence is biopsied.
RESULTS:
We present 3 representative cases in which occult lesions were identified with fluorescence visualization during longitudinal follow-up, resulting in the diagnosis of a primary dysplasia in case 1, a second primary cancer in case 2, and cancer recurrence in case 3.
CONCLUSIONS:
This is the first report of the diagnosis of occult oral disease using a simple noninvasive device. These early examples indicate the potential value of this technology to guide the management of patients with oral lesions, facilitating the detection of high-risk changes not apparent with white-light visualization.

Lane, Pierre M; Gilhuly, Terence; Whitehead, Peter; Zeng, Haishan; Poh, Catherine F; Ng, Samson; Williams, P Michele; Zhang, Lewei; Rosin, Miriam P; MacAulay, Calum E
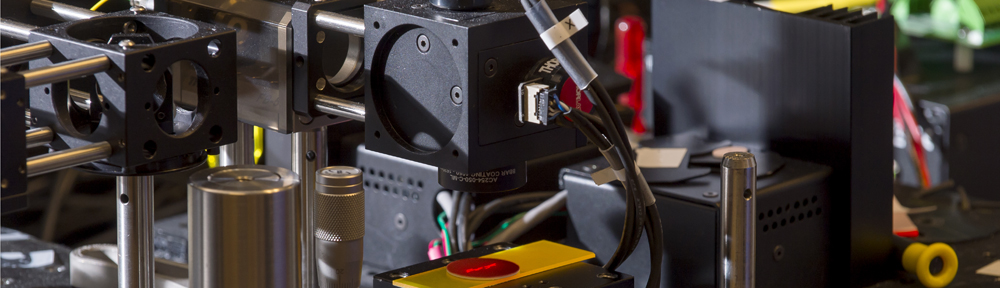
Simple device for the direct visualization of oral-cavity tissue fluorescence Journal Article
In: Journal of biomedical optics, vol. 11, no. 2, pp. 024006–024006, 2006.
@article{lane2006simple,
title = {Simple device for the direct visualization of oral-cavity tissue fluorescence},
author = { Pierre M Lane and Terence Gilhuly and Peter Whitehead and Haishan Zeng and Catherine F Poh and Samson Ng and P Michele Williams and Lewei Zhang and Miriam P Rosin and Calum E MacAulay},
url = {https://biophotonics.bccrc.ca/pubs/Lane-2006.pdf, Full Text (PDF)
http://www.ncbi.nlm.nih.gov/pubmed/16674196, PubMed},
doi = {10.1117/1.2193157},
year = {2006},
date = {2006-01-01},
journal = {Journal of biomedical optics},
volume = {11},
number = {2},
pages = {024006--024006},
publisher = {International Society for Optics and Photonics},
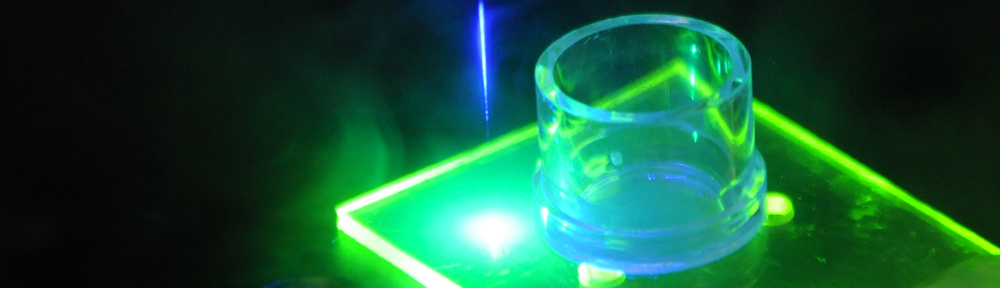
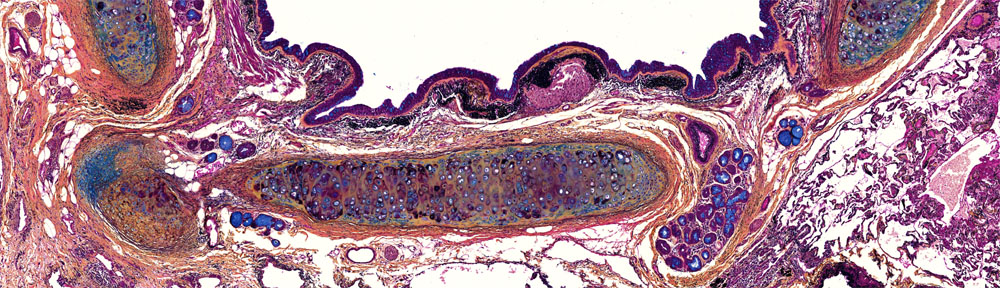
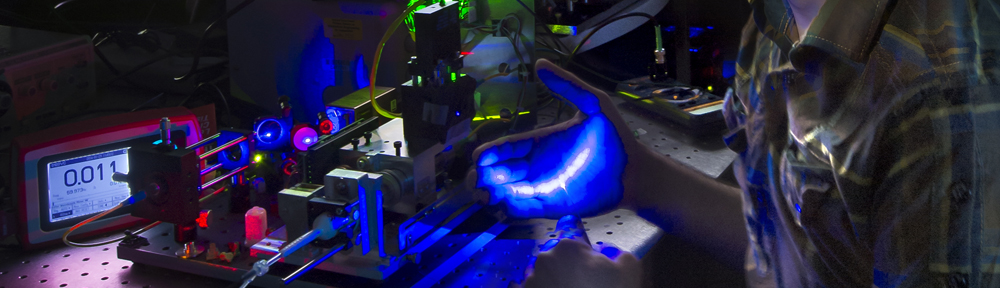
abstract = {Early identification of high-risk disease could greatly reduce both mortality and morbidity due to oral cancer. We describe a simple handheld device that facilitates the direct visualization of oral-cavity fluorescence for the detection of high-risk precancerous and early cancerous lesions. Blue excitation light (400 to 460 nm) is employed to excite green-red fluorescence from fluorophores in the oral tissues. Tissue fluorescence is viewed directly along an optical axis collinear with the axis of excitation to reduce inter- and intraoperator variability. This robust, field-of-view device enables the direct visualization of fluorescence in the context of surrounding normal tissue. Results from a pilot study of 44 patients are presented. Using histology as the gold standard, the device achieves a sensitivity of 98% and specificity of 100% when discriminating normal mucosa from severe dysplasia/carcinoma in situ (CIS) or invasive carcinoma. We envisage this device as a suitable adjunct for oral cancer screening, biopsy guidance, and margin delineation.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
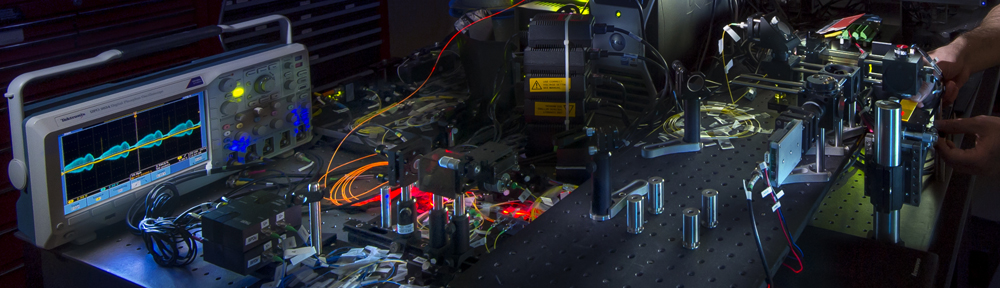
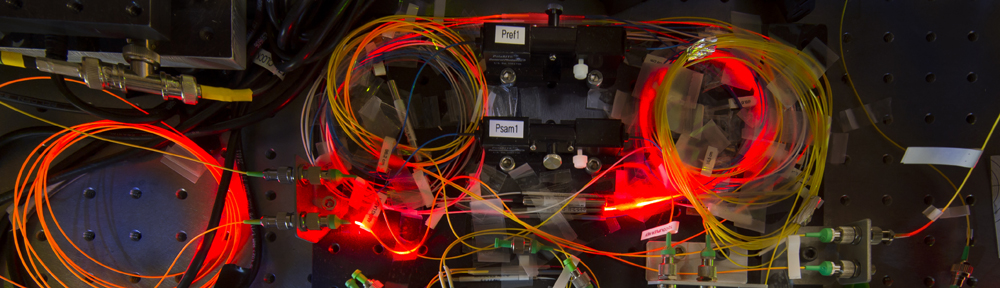
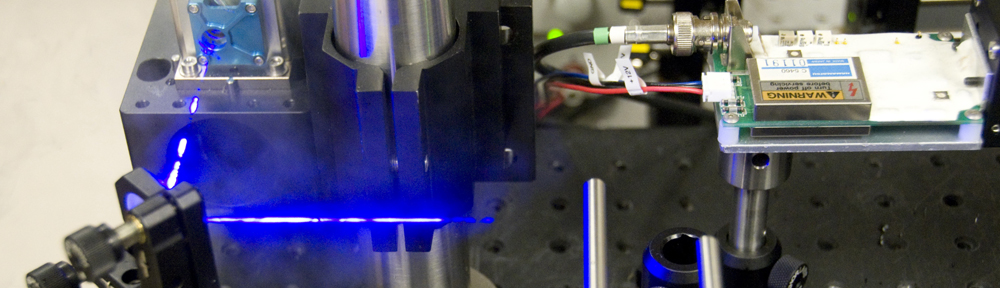
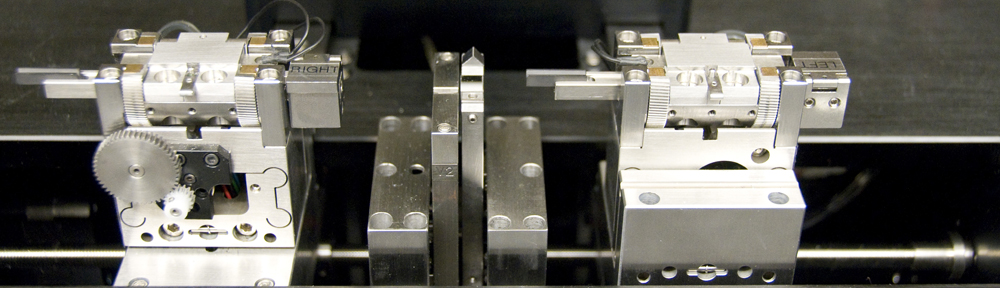
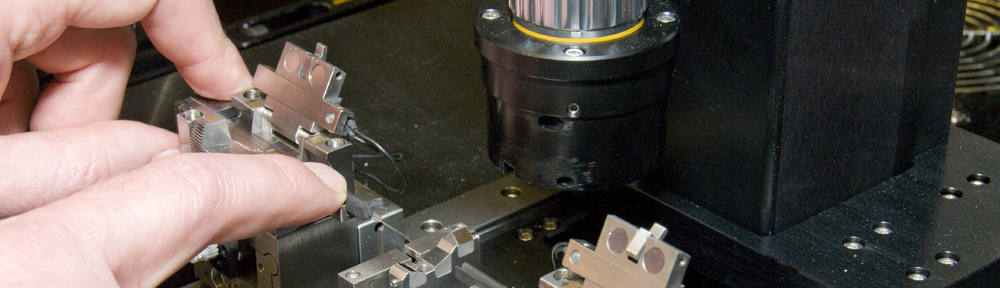
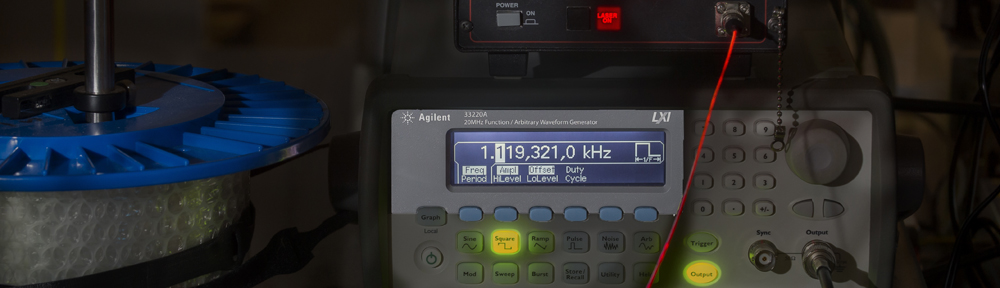
Early identification of high-risk disease could greatly reduce both mortality and morbidity due to oral cancer. We describe a simple handheld device that facilitates the direct visualization of oral-cavity fluorescence for the detection of high-risk precancerous and early cancerous lesions. Blue excitation light (400 to 460 nm) is employed to excite green-red fluorescence from fluorophores in the oral tissues. Tissue fluorescence is viewed directly along an optical axis collinear with the axis of excitation to reduce inter- and intraoperator variability. This robust, field-of-view device enables the direct visualization of fluorescence in the context of surrounding normal tissue. Results from a pilot study of 44 patients are presented. Using histology as the gold standard, the device achieves a sensitivity of 98% and specificity of 100% when discriminating normal mucosa from severe dysplasia/carcinoma in situ (CIS) or invasive carcinoma. We envisage this device as a suitable adjunct for oral cancer screening, biopsy guidance, and margin delineation.